Verify your patient is registered with the Programme
- Bowel cancer in Ireland
- Colorectal screening
- BowelScreen programme (also available for download: fact-sheet for health professionals)
- Eligible population
- The first round of BowelScreen
- BowelScreen home test - a faecal immunochemical test
- Advice about the size of the sample
- The BowelScreen journey
- BowelScreen surveillance guidelines
- Quality assurance measures
- About The National Screening Service
- Supporting evidence and further reading
Bowel cancer in Ireland
In Ireland, bowel (colon, rectal or colorectal) cancer is the second most common newly diagnosed cancer among people. Each year over 2,500 new cases of colorectal cancer are reported. The number of new cases is expected to increase significantly over the next 10 years, due mainly to an increasing and ageing population.
Colorectal cancer is currently the second most common cause of cancer death in Ireland.
Back to Top
Colorectal screening
The primary objective of colorectal cancer screening is to detect pre-cancerous adenomas in the lining of the bowel, thereby making colorectal cancer screening a truly preventative health measure.
This has the effect of potentially reducing the burden of treatment on both the individual and the health system. It reduces the stress, disruption and anguish that cancer diagnoses and subsequent treatment can bring to the individual, their family and community.
Back to Top
About the BowelScreen programme
The primary goal of BowelScreen – the national bowel screening programme, run by the National Screening Service (NSS), is to reduce mortality from colorectal cancer in people aged 55-74 in Ireland. A two page fact-sheet for health professionals about BowelScreen is available for download here.
The BowelScreen colorectal screening programme will offer free screening to people aged 55-74 on a two-yearly cycle. To develop capacity for the full population, the programme will be implemented on a phased basis, starting with people aged 60-69. Over 130,000 have already been invited since start of the programme (May 2014). This age group has the highest incidence of cancer within the wider age range. The maximum benefit in terms of reduction in mortality and cost-effectiveness will occur when the programme targets the full 55-74 age population.
Eligible people who indicate they wish to take part in the screening programme will be sent a screening test kit called a faecal immunochemical test (FIT). The test looks for the presence of blood, that is not visible to the eye, in the bowel motion.
The simple and easy-to-use test kit will include step-by-step instructions for self-administration of the test at home. The completed test can then be sent by Freepost to an accredited laboratory for analysis.
Approximately 94 per cent of people will receive a normal test result and will be sent another home test kit in two years’ time while they remain within the eligible age range.
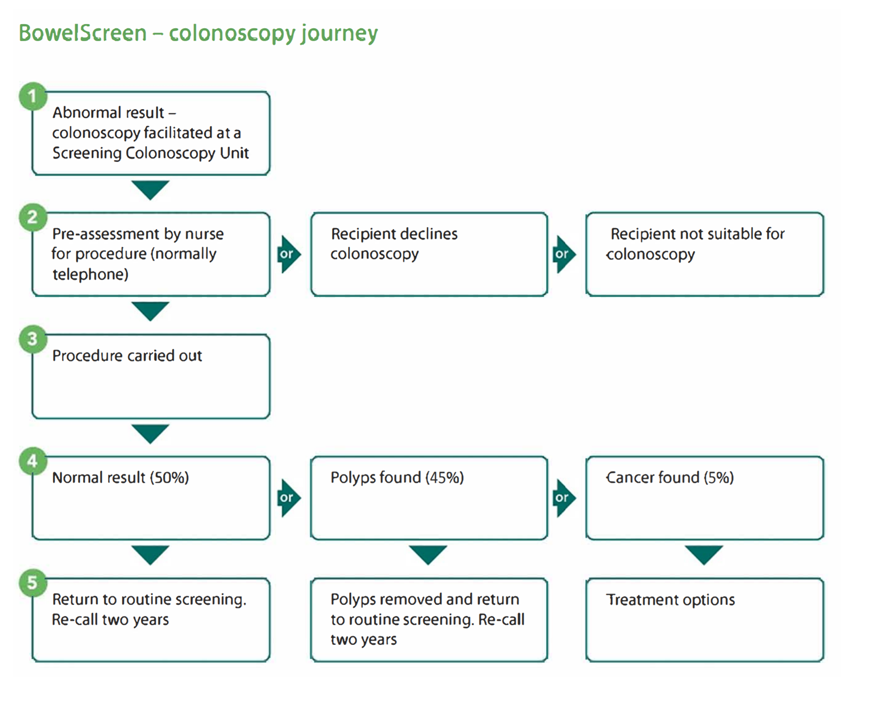
Five to six per cent of people will receive a not normal result following the home test kit and will require an additional test.
They will be offered a screening colonoscopy (an investigation of the lining of the bowel) at a hospital-based screening colonoscopy unit contracted by the NSS to provide this service.
Each person will be contacted by a nurse, who will assess the person’s suitability for colonoscopy and then guide them through the colonoscopy process. In the event that further treatment or surgery is required, defined pathways have been developed in conjunction with the National Cancer Control Programme (NCCP).
Each person will give their GP's details when they indicate they wish to take part in the programme. The GP will be sent copies of their client's correspondence with the BowelScreen programme - here is more information about the BowelScreen journey.
The NSS would like to express its continued appreciation for the role of GPs and the wider primary care community in supporting our screening programmes. With the support of the primary care community, the NSS is confident that BowelScreen can make a very real difference to the health of people in Ireland.
Back to Top
Eligible population
BowelScreen offers free bowel screening to people aged 59 to 70 every two years. Over time BowelScreen will be offered to those aged 55 to 74. BowelScreen puts together a register (list) of people eligible for screening from details supplied by the Department of Social Protection and self-registration.
If a person is currently in treatment for bowel cancer, does not have a colon or is not within the age range they are not offered free bowel screening as part of the BowelScreen programme.
Any person, regardless of eligibility for the BowelScreen programme who has any concerns or symptoms should see their GP (family doctor).
Back to Top
The first round of BowelScreen
BowelScreen has begun its first round of screening. The programme is being implemented on a phased basis, starting with offering free screening nationally to people aged 60-69 on a two-yearly cycle. As this is the first time the programme is being introduced, it will take up to three years for all eligible people to be invited. The programme will be expanded over time until the full 55-74 age group is reached.
The purpose of the screening programme is to identify the population most at risk of colorectal cancer and most likely to benefit from early detection and treatment. The maximum benefit in terms of reduction in mortality and cost-effectiveness will occur when the programme targets the full 55-74 age population.
An organised population-based screening for colorectal cancer is a complex and layered process. This programme is based on international evidence.
The programme is being introduced on a call, re-call basis. The current initial round of screening involves a number of steps including the identification of the target population, recruitment of the target population into the programme by a proactive call, delivery of a suitable screening test, analysis of the screening test, the re-call of people whose initial screening test indicates an abnormality and the provision of diagnosis and referral for treatment where required. A Freephone information line, materials and a comprehensive website support clients of the screening programme.
Back to Top
About the BowelScreen home test - a faecal immunochemical test
The programme uses the BowelScreen home test, a faecal immunochemical test (FIT) as its primary screening tool, which operates on an automated testing platform. This is one of the first international population-based screening programmes for colorectal cancer that utilises this technology as the primary screening tool. The FIT (also called the BowelScreen home test) is a simple test that looks for tiny amounts of blood, that are not visible to the eye, in the bowel motion.
One of the advantages of this test is that it can be self-administered in the privacy of the individual’s own home. For the vast majority (approximately 94 per cent) of the population, this will be the only test required. For a small minority (5 to 6 per cent), a further test (colonoscopy) at a hospital-based screening colonoscopy unit will be necessary.
The BowelScreen home test does not diagnose bowel cancer but it will tell whether a person needs further tests (a colonoscopy).
The date when the sample was taken must be written on the label on the plastic bag. It is important that the date is recorded accurately by the person taking the test as the sample needs to reach the laboratory within a set time period. If the date is not recorded the person may have to take the test again.
Back to Top
A small sample of your bowel motion is all that is needed. There is no need to provide a large sample of bowel motion.
Collect a small sample of your bowel motion, just enough to coat the end of the sampling stick, by scraping the sampling stick on your bowel motion (stool) until the end of the stick is completely covered.
Back to Top
The BowelScreen journey
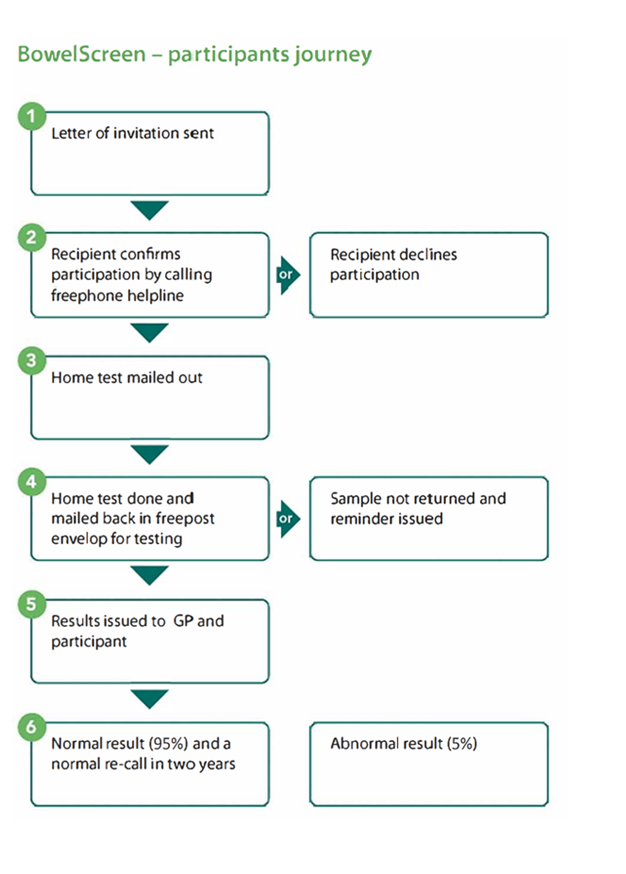
Back to Top
Quality assurance measures
In 2010, the NSS established a Quality Assurance committee, comprising of four subgroups - Programme and Administration; Endoscopy and Radiology; Histopathology; and Surgery. The members of each subgroup, who represent experts in each field, developed a set of quality assurance processes and standards for the national programme.
An International Peer Review Panel was convened in 2011 to examine the plans for the screening programme and the draft guidelines and to ensure the best of international evidence was incorporated into the process.
The work of the QA committee is now completed and the Standards for Quality Assurance in Colorectal Screening have been published. These guidelines will support the national colorectal screening programme.
A Clinical Advisory Group has been set up and supports the ongoing development of the programme and provides ongoing clinical advice to the NSS.
Back to Top
About The National Screening Service
The National Screening Service (NSS) is part of the Health Service Executive.
The National Screening Service aims to maximise expertise and learning across population-based screening programmes and improve efficiencies by developing a single governance model for screening. It currently encompasses BreastCheck – The National Breast Screening Programme, CervicalCheck – The National Cervical Screening Programme and Diabetic RetinaScreen - The National Diabetic Retinal Screening Programme.
As with BreastCheck, CervicalCheck and Diabetic RetinaScreen , the NSS ensures that quality assurance is paramount and all the essential elements are in place to ensure risks to patients are minimised and that the best clinical outcomes for patients are maximised.
Back to Top
Supporting evidence and further reading
A list of some references and further reading has been compiled, yet is not exhaustive. Most references can be downloaded by clicking on the links below:
Guidelines for Quality Assurance in Colorectal Screening
Source: The National Cancer Screening Service Quality Assurance Committee for Colorectal Screening
European guidelines for quality assurance in colorectal cancer screening and diagnosis - First Edition
Source: ISBN 978-92-79-16435-4 (14 Nov 2011)
Segnan N, Patrick J, von Kara L (eds), 2010
The UK colorectal cancer screening pilot: results of the second round of screening in England
Source: British Journal of Cancer (2007) 97, 1601 - 1605
By: D Weller, D Coleman, R Robertson, P Butler, J Melia, C Campbell, R Parker, J Patrick, S Moss
Outcomes of the Bowel Cancer Screening Programme (BCSP) in England after the first one million tests
Source: Gut 2012:61 1439-1446. doi:10.1136/gutjnl-2011-300843
By: R F A Logan, J Patnick, C Nickerson, L Coleman, M D Rutter, C von Wagner, on behalf of the English Bowel Cancer Screening Evaluation Committee
Comparison of a guaiac based and an immunochemical faecal occult blood test in screening for colorectal cancer in a general average risk population
Source: Am J Gastroenterol (2010) September 105 (9): 2017-27; E Pub 2010 May 25
By: L Guittet, V Bouvier, N Mariotte, JP Vallee, D Arsene, S Boutreux, J Tichet, G Launoy
Random Comparison of Guaiac and Immunochemical Fecal Occult Blood Tests for Colorectal Cancer in a Screening Population
Source: Gastroenterology 2008; 135:82-90
By: L van Rossum, A van Rijn, R J Laheij, M G van Oijen, P Fockens, H H van Krieken, A L Verbeek, J B Jansen, E Dekker
Interventions to Increase the Uptake of Cancer Screening: Guideline Recommendations
Source: Cancer Care Ontario, Draft Report, March 26 2009
By: M Brouwers, C De Vito, A Carol, J Carroll, M Cotterchio, M Dobbins, B Lent, C Levitt, N Lewis, SE McGregor, L Paszat, C Rand and N Wathen; A quality initiative of the Cancer Screening Uptake Expert Panel, Cancer Care Ontario and the Program in Evidence-Based Care (PEBC), Cancer Care Ontario (CCO)
Back to Top